10 Pulmonary Capillaries and Nonventilatory Function
Learning objectives
- Describe the factors that determine fluid movement between the pulmonary circulation and airspaces and how these may change to produce pulmonary edema.
- Describe nonventilatory roles of the pulmonary circulation.
Introduction
The gas exchange surface needs fluid on both the alveolar side and the capillary side for gases to dissolve into solution so they can be transported. Controlling the level of fluid on the internal alveolar surface is paramount and requires a balance between several forces. We will look at these forces here. We will also look at some of the nonventilatory roles of the lung. As the recipient of all cardiac output and with an architecture that provides a large surface area, the lung is well positioned to play other metabolic roles.
Pulmonary Capillaries and Fluid Exchange
Before looking at the unique situations that influence movement of fluid into and out of the capillary and alveoli, we will briefly review the usual Starling’s forces that influence fluid movement between a capillary and the surrounding tissue.
First we will look at the balance of hydrostatic forces across the walls of a capillary as it travels through tissue. Being closest to the pumping heart, the hydrostatic pressure at the arterial end is relatively high, and likely much higher than the hydrostatic force in the interstitial space. This forms a hydrostatic pressure gradient that water moves down and out of the capillary into the tissue.
This exit of water from the capillary leaves behind a greater concentration of plasma proteins. This causes the colloid osmotic pressure to progressively rise down the capillary, and thus begins to establish an osmotic gradient with a tendency to drag water back into the capillary from the tissue. This, and the progressive drop in capillary hydrostatic pressure due to the fluid loss to the tissue and increasing distance from the heart, means most of the exuded fluid returns back to the capillary at the venous end down a hydrostatic and osmotic gradient.
The only other variable to consider here is the permeability of the capillary’s endothelium and other membranes. Pulmonary capillaries are continuous and therefore normally leak relatively little, but exposure to toxins or inflammatory mediators can cause permeabilization of the capillary endothelium and increase outward fluid movement, just like a capillary in the systemic circulation.
Unlike the systemic capillaries, though, the pulmonary capillaries are exposed to airway and alveolar forces that can influence fluid movement.
Alveolar surface tension caused by the fluid lining of the internal alveolus wall not only drags the alveolar walls inward, but can also cause entry of fluid from the capillary and interstitium into the airspace. Excessive fluid accumulation can produce interstitial or alveolar edema, edema in the alveoli being much more serious as it interferes with gas exchange.
Nonrespiratory Functions of the Pulmonary Circulation
Because all cardiac output travels through the pulmonary circulation, it is ideally suited to host the enzymes needed to perform metabolic functions on blood components.
We will deal with only a few here as it is more effective to address each metabolic pathway in context of its function, rather than merely because of the location in which it occurs.
ACE: Perhaps the lung’s most well-known metabolic role is to host the angiotensin-converting enzyme (or ACE). This enzyme is responsible for converting angiotensin I (released during periods of hypotension) to angiotensin II, a powerful vasoconstrictor that helps raise blood pressure. The same enzyme also inactivates 80 percent of circulating bradykinin (a potent vasodilator).
Serotonin: Other circulating substances that are controlled by the lung include serotonin, as the lung is the major site for removing serotonin from the circulation. The lung stores the serotonin, rather than breaking it down, and even transfers it to platelets who use serotonin in their hemostatic role.
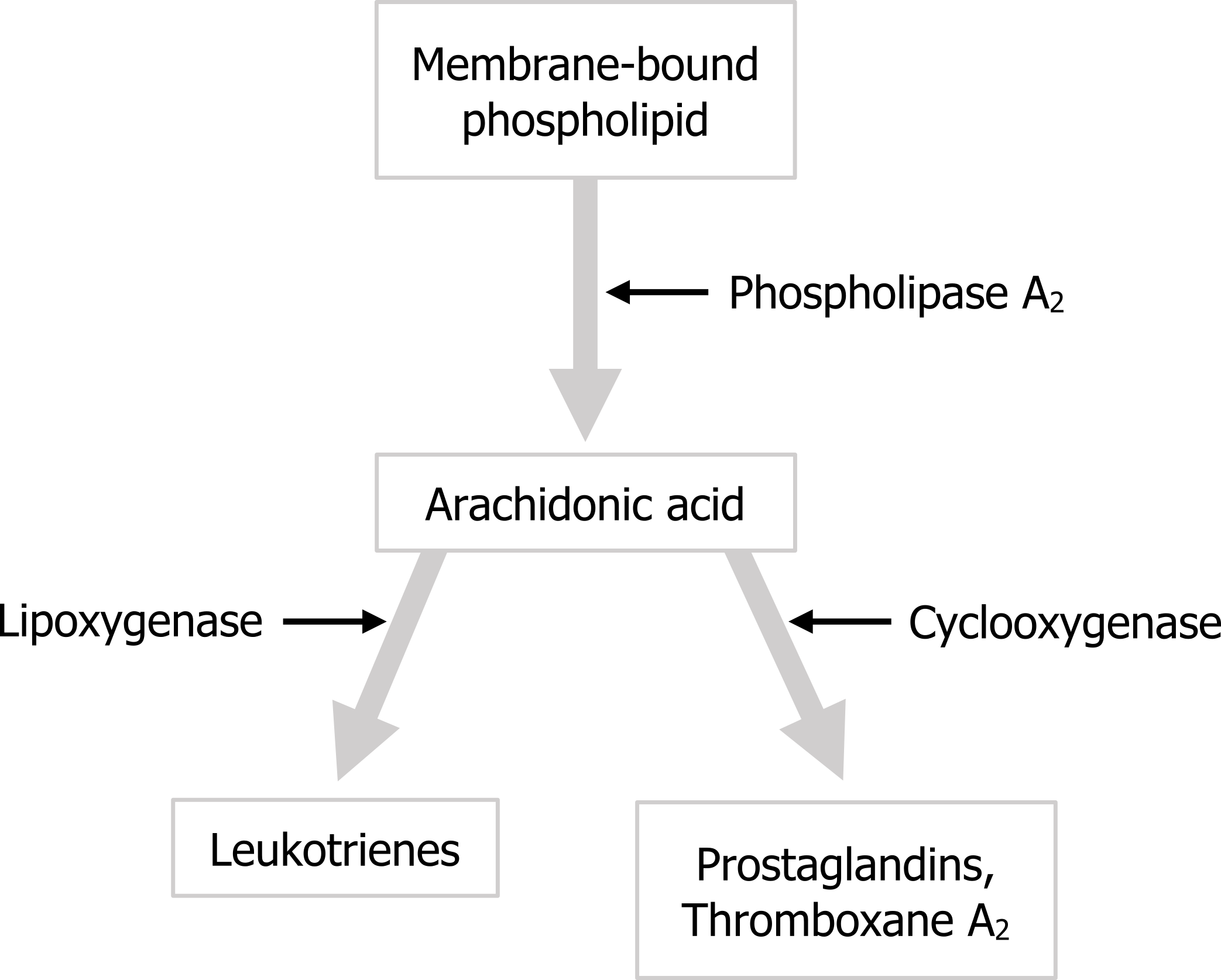
Arachidonic acid: The lung is also involved in the metabolism of arachidonic acid, which is worth dealing with here as well because not only are the products of this metabolism vasoactive, they can also influence airway smooth muscle and cause bronchoconstriction. In brief, arachidonic acid is produced by the action of a phospholipase on membrane-bound phospholipids. The arachidonic acid can then follow one of two pathways (figure 10.1): to produce leukotrienes, which are involved in the inflammatory response and can cause bronchoconstriction, or to produce prostaglandins and thromboxane through the action of cyclooxygenases. The relevance for us here is that these alternative pathways explain why some asthmatics are sensitive to aspirin and bronchoconstrict when they take aspirin. Aspirin inhibits cyclooxygenase and thus blocks one of these pathways. Consequently there is more substrate, arachidonic acid, available for the alternate pathway and so more leukotrienes are produced, in response to which the hypersensitive airways of the asthmatic bronchoconstrict.
Summary
So from this chapter you should be able to determine the direction of fluid movement into and out of the pulmonary capillaries given the Starling and lung forces involved, and appreciate that the lung plays other relatively small but significant metabolic roles.
References, Resources, and Further Reading
Text
Levitsky, Michael G. “Chapter 10: Nonrespiratory Functions of the Lung.” In Pulmonary Physiology, 9th ed. New York: McGraw Hill Education, 2018.
West, John B. “Chapter 4: Blood Flow and Metabolism—How the Pulmonary Circulation Removes Gas from the Lung and Alters Some Metabolites.” In Respiratory Physiology: The Essentials, 9th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams and Wilkins, 2012.
Figures
Figure 10.1: Pulmonary metabolism of arachidonic acid. Grey, Kindred. 2022. CC BY 4.0. https://archive.org/details/10.1_20220125

