4 Distribution of Ventilation
Learning objectives
- Describe the distribution of ventilation and how it is affected by gravity and lung volume.
Radial Traction
Introduction
Taking a breath in one might imagine that each part of the lung gets an equal share of the inspired air. But regions of the lung are not equally ventilated. The unequal distribution is caused by (1) gravity and (2) lung volume.
Lung Parenchyma and Radial Traction
Before we look at ventilation distribution we need to understand a little more about lung structure. Although the lung is composed of individual components, such as the alveoli within distinct ascini, the airways, and the blood vessels, the parenchymal tissue between these components helps form the mechanical structure of the lung.
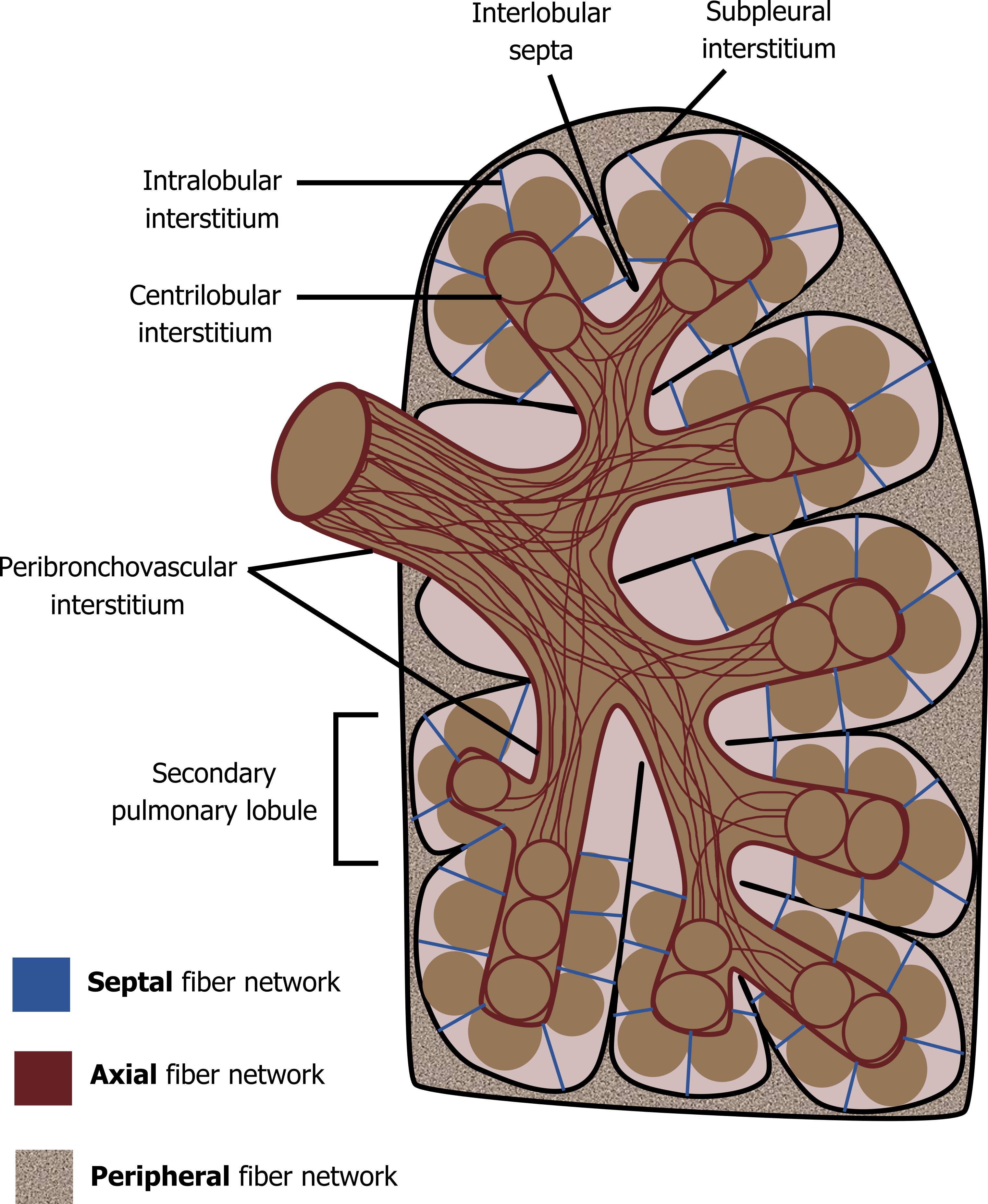
In brief, collagenous and elastic fibers run the length of the large airways and into the lobes forming the axial network. Fibers beneath the pleura and within the septal spaces between the lobes form a peripheral network, and finally thin fibers surrounding the alveoli within the lobes form the septal network. Together these networks form a fibrous “web” of the lung (figure 4.1).
Functionally what this means is that movement of one lung structure is transferred to others. As the lung inflates these fibrous connections have a significant impact on lung function and the pulmonary vasculature. Expanding alveoli pull on fibers that are attached to neighboring airways and blood vessels and, indeed, other alveoli.

The expanding lung volume tends to pull open airways and blood vessels, lowering the resistance of both as inspiration continues, as is illustrated in figure 4.2.
Radial traction (sometimes called parenchymal traction) is an important component of the lung’s mechanical behavior, and it means that lung volume has an effect on airway and vascular resistance.
More important for us now though is the understanding that the lung is highly connected within itself. And it is a good thing that it is these fiber networks transfer changes in pleural pressure from the lung periphery to its center; without the networks, only the alveoli at the periphery of the lung would expand when pleural pressure became negative during inspiration.
It also means that the effects of gravity are transferred to the lung as a single unit, and we will look at that now.
Distribution of Ventilation Across the Lung
Introduction
The lung hangs in the thorax supported by the trachea and the surface tension adhering its outer surface to the inside of the thoracic cavity. Gravity obviously tends to pull the lung downward, and this pull has an unequal effect on alveoli at different heights of the lung.
Distribution of Ventilation and Gravity
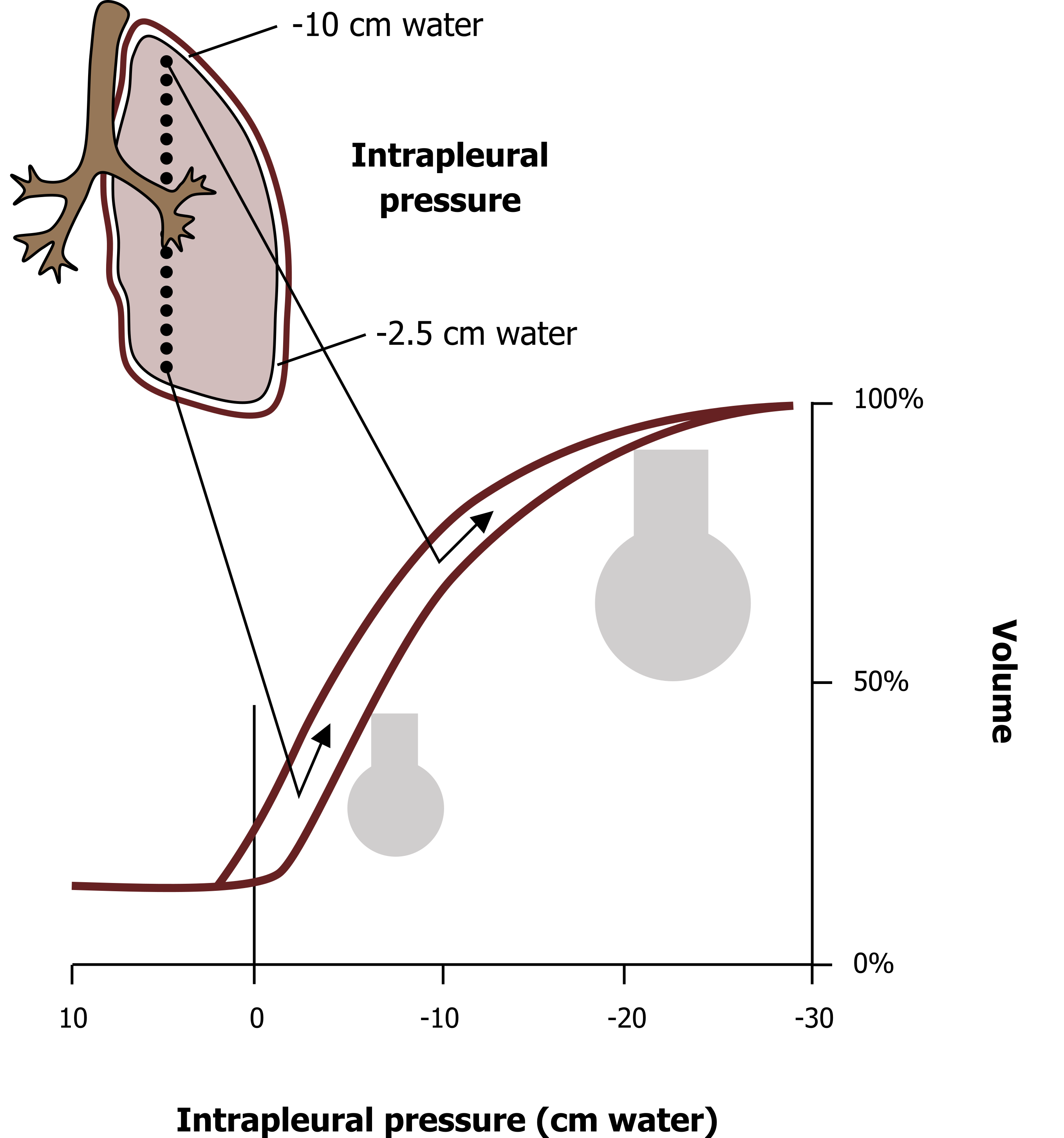
Alveoli at the apex (top) of the lung have a substantial amount of lung tissue below them for gravity to act on, so there is a large force pulling the lung away from the pleural space here and hence at the top of the lung intrapleural pressure is more negative. As we descend down the lung the mass below each point becomes less and less, so the pull on the pleural space declines, and we see intrapleural pressure become less and less negative.
Simply because of gravity, therefore, we have a distribution of intrapleural pressures. As you know from the previous chapter, intrapleural pressure determines alveolus size (figure 4.3). So at the apex of the lung alveoli tend to be large because of the more negative intrapleural pressure, while at the base, alveoli are less extended because of the less negative intrapleural pressure. If an analogy would help, look at this slinky being held up (figure 4.4). The coils near the top of it are pulled far apart because of the weight of the slinky below the top. As you travel down the slinky the coils are less and less extended as less and less weight below pulls on them. The lung acts just the same; alveoli at the top are extended at rest, while those at the base have a smaller volume.
This has ramifications on where air entering the lung goes and how ventilation is distributed across the lung (more on the implications of this in chapter 13). Alveoli at the apex of the lung are already extended and therefore have limited capacity to take in more air; their resting volume is also close to the flat part of the compliance curve (figure 4.3), so they are more difficult to inflate. The smaller alveoli at the base of the lung, however, still have a greater capacity for expansion, and the smaller resting volume places them on the steeper section of the compliance curve; consequently they are easier to inflate, and air takes the path of least resistance.
Because of this, the alveoli at the apex of the lung rapidly fill to capacity on inspiration, and the vast majority of inspired air descends toward the base toward the more compliant and less extended alveoli. This uneven distribution of ventilation is something we will return to when we address other learning objectives, so it is worth understanding.
Distribution of Ventilation and Lung Volume
The distribution of ventilation is also effected by lung volume, and at low lung volumes the apex of the lung is actually better ventilated than the base—again, this is due to changes in alveolar compliance.
As the lung is emptied below functional residual capacity, that is below the normal point that expiration ends, the recoil of the lung is reduced and therefore intrapleural pressure becomes progressively less negative (or more positive if that is the way you would like to think of it). Compared to the normal resting volume we just dealt with, at low lung volumes the intrapleural pressure may be up to −4 cm H2O (compared to −10). This pushes the apical alveoli down on to the steep part of the compliance curve, and therefore they are easier to inflate.
The intrapleural pressure at the base of the lung may actually become positive at low lung volumes. Now that force that tended to open up alveoli is actually a force that tends to compress alveoli. In our example here the intrapleural reaches 3.5 cm H2O, a force that may lead to airway compression and thereby reduce ventilation to the basal alveoli. This intrapleural pressure will certainly place these alveoli on the very flat and therefore noncompliant section of the compliance curve and make them difficult to inflate because of the surface tension and small radius effect we have discussed previously.
Summary
Ventilation is unevenly distributed across the lung because of the range of intrapleural pressures that are established down the lung by gravity. At normal lung volumes the base of the lung is better ventilated than the apex.
At low lung volumes this relationship is reversed as intrapleural pressures at the base of the lung become compressive, reducing the compliance of basal alveoli, while the compliance of apical alveoli is increased.
References, Resources, and Further Reading
Text
Levitsky, Michael G. “Chapter 2: Mechanics of Breathing.” In Pulmonary Physiology, 9th ed. New York: McGraw Hill Education, 2018.
West, John B. “Chapter 7: Mechanics of Breathing—How the Lung Is Supported and Moved.” In Respiratory Physiology: The Essentials, 9th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams and Wilkins, 2012.
Widdicombe, John G., and Andrew S. Davis. “Chapter 1.” In Respiratory Physiology. Baltimore: University Park Press, 1983.
Figures
Figure 4.1: The fiber networks of the lung. Grey, Kindred. 2022. CC BY 4.0. https://archive.org/details/4.1_20220125/mode/1up
Figure 4.2: The action of radial traction. Grey, Kindred. 2022. CC BY 4.0. https://archive.org/details/4.2_20220125/mode/1up
Figure 4.3: Interaction of lung volume, compliance, and distribution of ventilation. Grey, Kindred. 2022. CC BY 4.0. https://archive.org/details/4.3_20220125/mode/1up
Figure 4.4: Lung = slinky. Binks, Andrew. 2022. CC BY-NC-SA 4.0.

