2 Upper Airway Infections
Learning objectives
- List the common viral and bacterial agents associated with upper airway infections.
- Describe the pathological events associated with an upper airway infection and how it may progress into other regions of the respiratory tract.
While the most prevalent upper respiratory tract infection (URI) is the self-limited “common cold,” other less frequently occurring forms can have more serious consequences. Differentiating between the “common cold” and more consequential infections is therefore a clinical goal.
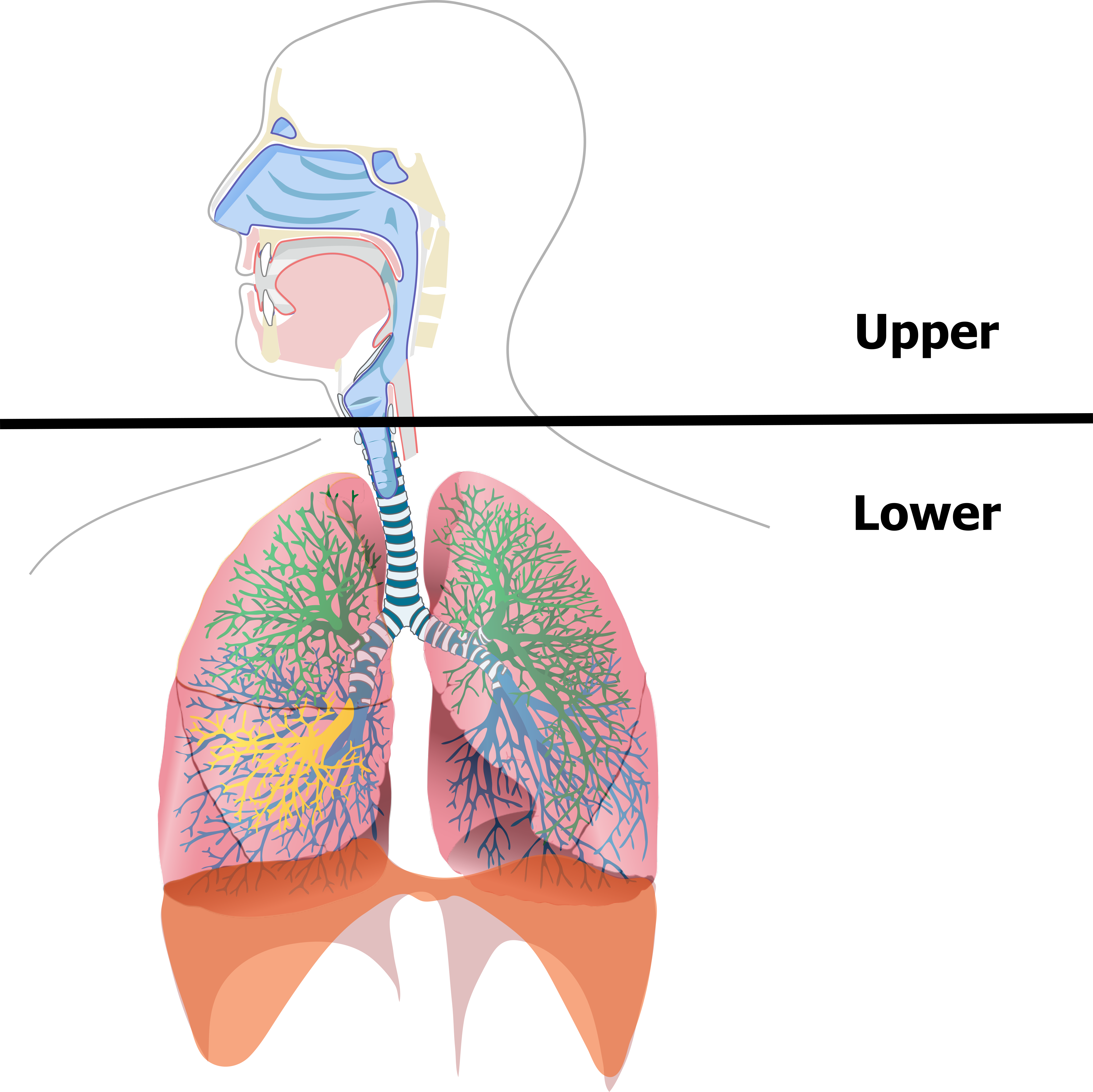
First, a quick reminder of the region we are talking about. The upper airway encompasses the extrathoracic respiratory tract, so includes the nasal cavity, paranasal sinuses, pharynx, and sometimes the larynx (figure 2.1). The lower airway starts from the trachea and includes all downstream structures.
The Common Cold
As with most URIs the common cold is caused by a viral infection, and although there are several different viral candidates for causing a common cold, the pathophysiological mechanism and symptoms are the same regardless of the type. This is because it is the innate immune response, rather than the direct infection, that is responsible for most of the symptoms.
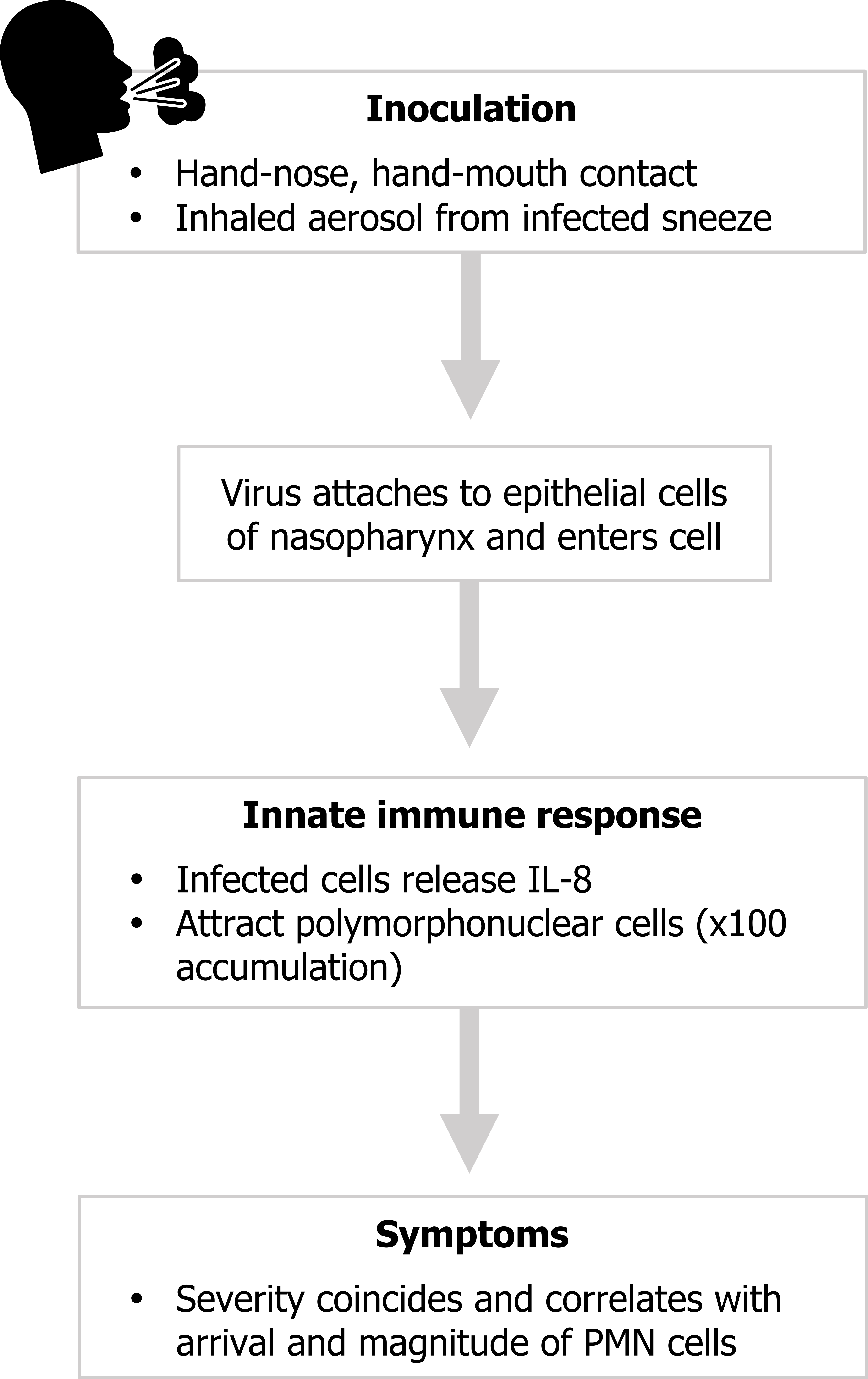
Looking at the sequence of events involved in “getting a cold” (figure 2.2), we start with delivery of the pathogen to the upper airway and inoculation. The most common modes of delivery are hand-to-nose or hand-to-mouth contact or inhalation of aerosolized nasal fluid produced from a sneeze of an infected person. The causal virus is rarely found in saliva, so infection is spread from snot not spit.
Once in the upper airway, and if the pathogen can breach the innate defenses here (mucus and the mucociliary escalator), the virus attaches to, and then enters, the epithelial cells. In response, the invaded epithelial cells release cytokines to instigate an immune response. The primary cytokine released in this scenario is IL-8, which causes the attraction and accumulation of polymorphonuclear cells (PMN).
It is the substantial increase in PMN cells that is responsible for most of the symptoms of a common cold—runny nose, postnasal drip, and other signs of epithelial inflammation.
By far the most common cause of the common cold is the rhinovirus, followed by coronavirus and influenza, then less frequently by parainfluenza respiratory syncytial virus (RSV), and then rarely by adenovirus or enterovirus (table 2.1).
| Virus | Estimated proportion in common cold | Spring | Summer | Fall | Winter |
|---|---|---|---|---|---|
| Rhinovirus | 30-50% | Yes | Yes | ||
| Coronavirus | 10-15% | Yes | |||
| Influenza | 5-15% | Yes | Yes | ||
| Parainfluenza | 5% | Yes | |||
| Respiratory syncytial virus | 5% | Yes | Yes | ||
| Adenovirus | <5% | Yes | Yes | Yes | Yes |
| Enterovirus | <5% | Yes | Yes |
Table 2.1: The viral pathogens.
Seasonal differences (table 2.1) in the prevalence of these pathogens might help you identify the causal agent, but as the viral infections are self-limiting it is more important to ensure there is no bacterial involvement.
A viral infection can progress and cause more specific conditions than a cold, and these are identified by their location.
Rhinosinusitis
Rhinosinusitis is most commonly caused by a viral infection, and despite popular belief is only rarely associated with a concurrent bacterial infection in adults. The lining of the nasal and sinus cavities becomes inflamed, again as a result of the immune response rather than a direct effect of the virus. The congestion can be painful, but symptoms can be treated with over-the-counter analgesics. Like the common cold, the condition is self-limiting and normally resolves in seven to ten days.
Pharyngitis
When the pharynx is involved the local inflammation will cause the patient to present with a sore throat and a hoarse voice. Pharyngitis is most commonly caused by viral infection, but more serious bacterial infections (e.g., Streptococcus) should be considered. The two infection types are easily distinguished with tonsillar exudate and petechial mottling of the soft palate being present in a bacterial infection, but absent in a viral infection. Treatment of viral pharyngitis is limited to symptom relief, and antibiotics should be avoided.
Viral Croup
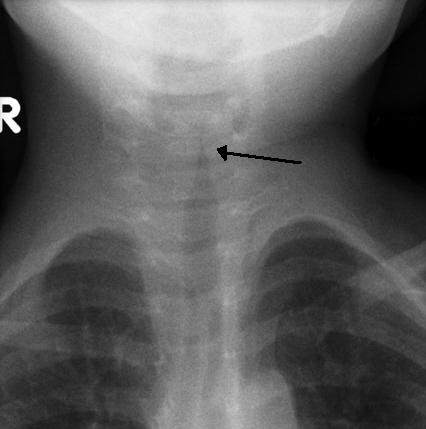
Involvement of the larynx and subglottic airway will produce croup. There are numerous causes of croup and subclassifications depending on the region involved. Viral croup, like other forms, involves inflammation of the larynx that causes the airway to narrow. Edematous airway walls form an upper airway obstruction that produces stridor. Stridor is a crow-like airway sound, and the phase of breathing that it appears in can be helpful in determining the site of obstruction. Stridor during inspiration is indicative of airway collapse above the vocal cords (i.e., extrathoracic), and expiratory stridor suggests a tracheal or bronchial obstruction (i.e., intrathoracic). The constriction of the airway can be seen on x-ray when severe and the narrowing produces a characteristic “steeple” sign in the trachea (see figure 2.3).
Bacterial Infection of the Upper Airway
The induction of upper airway infection by bacteria is similar to that by virus with droplet inhalation or hand-to-mouth or nose contact. Cell adherence is usually promoted by bacterial properties, but it is bacterial toxins that instigate the signs and symptoms of infection rather than the innate immune system. We will now cover four bacteria that are capable of causing an upper airway infection.
Group A Streptococcus

The pathogenic mechanisms of Group A Streptococcus are poorly understood—partly because of the numerous and complex ways it interacts with its human host. Its coat protects it from phagocytosis, antibody binding, and opsonization. It is capable of releasing a cocktail of cell-lysing toxins as well as pyrogenic exotoxins that:
- induce lymphocyte production,
- suppress antibody synthesis, and
- induce fever.
In terms of the upper airway it is the leading cause of tonsillopharyngitis in both adults and children. A sore throat may be accompanied by fever, headache, and vomiting. Inflamed tonsils and uvula may be coated in exudates, and palatal petechiae (figure 2.4) may be be present as well as a scarlatiniform rash. Symptoms resolve in three to five days, but antibiotic therapy should be used to reduce the risk of complications that include peritonsillar cellulitis, otitis media, sinusitis, and even acute rheumatic fever.
Corynebacterium diphtheriae

After inoculation, C. diphtheriae releases diphtheria exotoxin and enters the cell by exploiting a membrane receptor. Once inside, the exotoxin inactivates elongation factor 2, halting protein production and causing cell death. Occurrence of diphtheria is now rare in developed countries because of vaccination programs, but infection produces sore throat, swelling of cervical lymph glands, and low-grade fever. Most cases are tonsillopharyngeal where a pseudomembrane and exudate (figure 2.5) is produced that can spread to other areas. In severe cases the spread can lead to the bull neck of diphtheria (figure 2.5) as swelling and pseudomembranes accumulate and swallowing can become difficult. If the infection becomes systemic, cardiac, neural, and renal issues may arise, including myocarditis, local neuropathies, and in severe cases renal failure.
Bordetella pertussis
After inhalation, B. pertussis attaches to airway cells through a variety of adhesion molecules. The organism then releases cytotoxins that cause loss of protective respiratory cells and promote microaspiration and a distinct and prolonged cough. Pertussis’s nickname of whooping cough comes from the distinct inspiratory noise. The paroxysmal stage of pertussis (that involving cough) can last between two and ten weeks, and this prolongation is likely due to the bacteria penetrating deeper regions of the lung (the cytotoxins have been found in alveolar macrophages). The disease can be life threatening to infants, but widespread vaccinations started in the forties dramatically reduced its incidence.
Haemophilus influenzae
The outer coat of the H. influenzae contains several proteins that attach to upper airway cells and specifically promote pharyngeal and the middle ear colonization. The outer coat also acts as an endotoxin and elicits a potent inflammatory response to produce the symptoms of the infection. Prior to routine vaccination, vascular invasion by the pathogen could produce metastatic foci including meningitis, septic arthritis, osteomyelitis, and cellulitis. Today, while upper airway infection can lead to pneumonia, the incidence of bacteremia is low.
References, Resources, and Further Reading
Text
Thomas, Micah, and Paul A. Bomar. Upper Respiratory Tract Infection. Treasure Island, FL: StatPearls Publishing, 2022. https://www.ncbi.nlm.nih.gov/books/NBK532961, CC BY 4.0.
Figures
Figure 2.1: The upper airway encompasses the respiratory tract above the trachea. Grey, Kindred. 2022. CC BY 4.0. Includes Respiratory system complete en by LadyofHats from WikimediaCommons (public domain). https://archive.org/details/2.1_20220203
Figure 2.2: Pathophysiology of the common cold. Grey, Kindred. 2022. CC BY 4.0. Added flu by Vectorstall from Noun Project (CC BY 3.0). https://archive.org/details/2.2_20220203
Figure 2.3: An x-ray of the upper airway of a child suffering from tracheal croup. Gaillard, Frank. 2010. CC BY-SA 3.0. “Croup Steeple Sign” from WikimediaCommons.
Figure 2.4: Typical signs of “strep throat.” Heilman, James. 2010. CC BY-SA 3.0. “Pos Strep” from WikimediaCommons.
Figure 2.5: Clinical signs of c. diphtheriae: pseudomembrane exudate (upper), and bull-neck (lower). Grey, Kindred. 2022. CC BY-SA 3.0. Added Dirty white pseudomembrane classically seen in diphtheria 2013-07-06 11-07 by Dileepunnikri from WikimediaCommons (CC BY-SA 3.0) and Diphtheria bull neck.5325 lores by CDC from WikimediaCommons (public domain). https://archive.org/details/2.5_20220203

