3 Lower Airway Infections
Learning objectives
- Describe three types of lower airway infection and their pathophysiology.
- Categorize pneumonia on a histological, anatomical, and etiological basis.
- List the clinical findings associated with pneumonia.
Despite being open to the external environment, lower airway infections are relatively rare because of the lungs, multitiered defense systems. However, these defenses can be breached if they are weakened or the presentation of a pathogen is overwhelming.
The site of the infection in the lower airways determines the form and severity of the disease. Infection of the trachea and bronchi produces acute bronchitis. Deeper into the airways and the infection produces acute infectious bronchiolitis, and deeper still, when infection reaches the air ducts and alveoli, we have pneumonia. Because pneumonia involves the gas exchange surfaces these infections tend to be most severe, and consequently we will spend most of this chapter on them. But first we will look at acute bronchitis and acute infectious bronchiolitis.
Acute Bronchitis
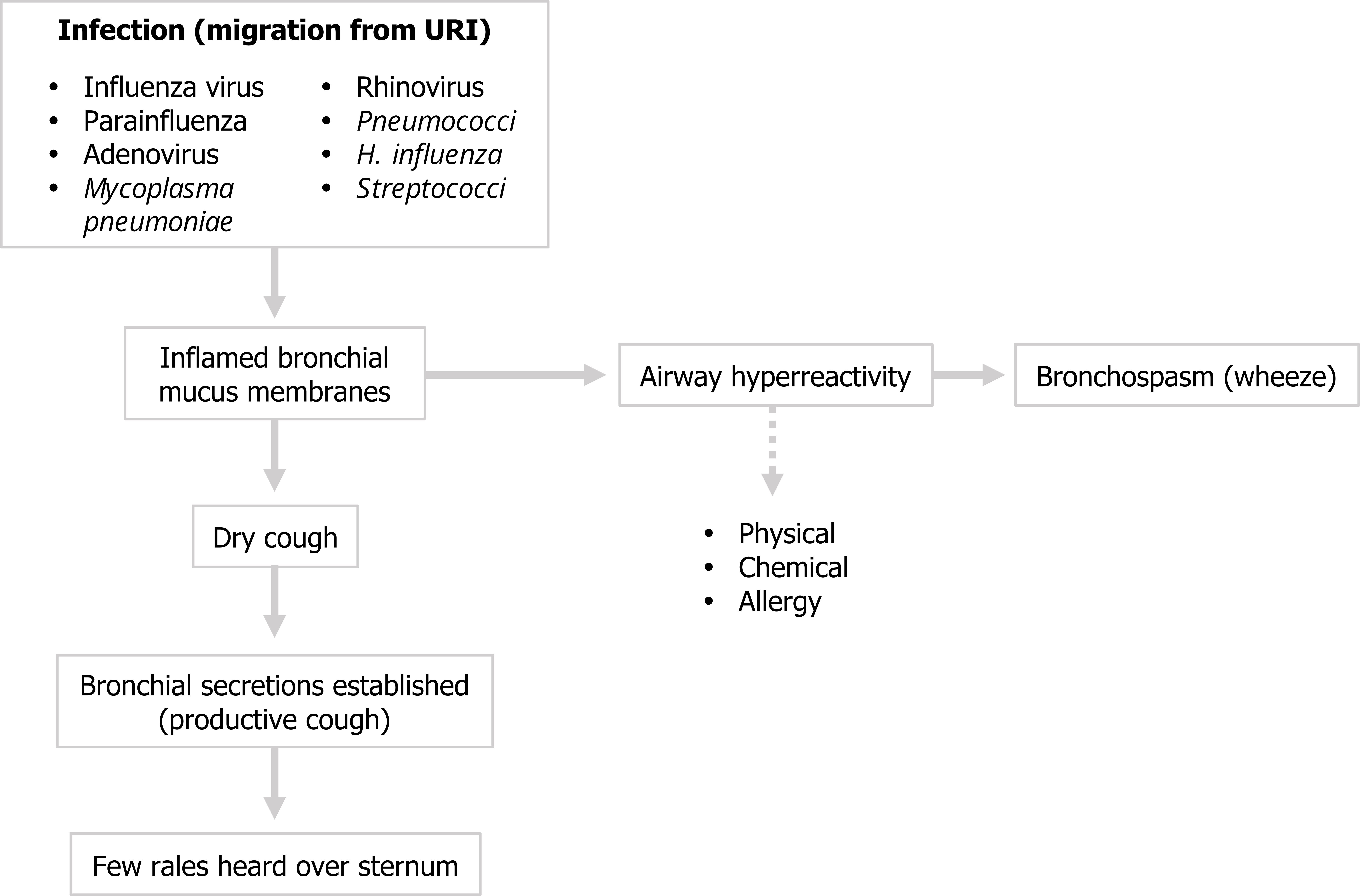
Acute bronchitis often originates from a migrating upper airway infection, and hence the usual candidates for a URI are the pathogens associated with acute bronchitis, and most are viral but can include mycoplasma infection. Acute bronchitis can be caused by bacteria, but it is usually an opportunistic secondary infection by resident bacteria taking advantage of a weakened airway. Regardless of the pathogen, let us look at the sequence of pathophysiological events in acute bronchitis (figure 3.1).
First the bronchial mucus membranes become inflamed. Taking a careful history can help you distinguish infectious causes from other instigators of airway inflammation, such as physical or chemical insults or an allergic response. The inflammation will initially produce a dry cough, but within two to three days bronchial secretions will be established, the cough will become productive, and rales can be heard over the site of the infection, which constitutes the clinical diagnosis.
The inflamed airways may also become hyperreactive, and this may compound any concurrent allergic response or existing asthma resulting in bronchospasm and wheeze. See figure 3.1 for a summary.
Infectious Bronchiolitis
Penetrating deeper into the airway a pathogen can cause acute infectious bronchiolitis. By far the most common culprit is respiratory syncytial virus (RSV). This is the most common cause of lower airway infection in children under one year old and is estimated to cause more infant deaths than any other pathogen with the exception of malaria. While it can affect adults, it usually occurs only in the elderly and immunosuppressed patients.
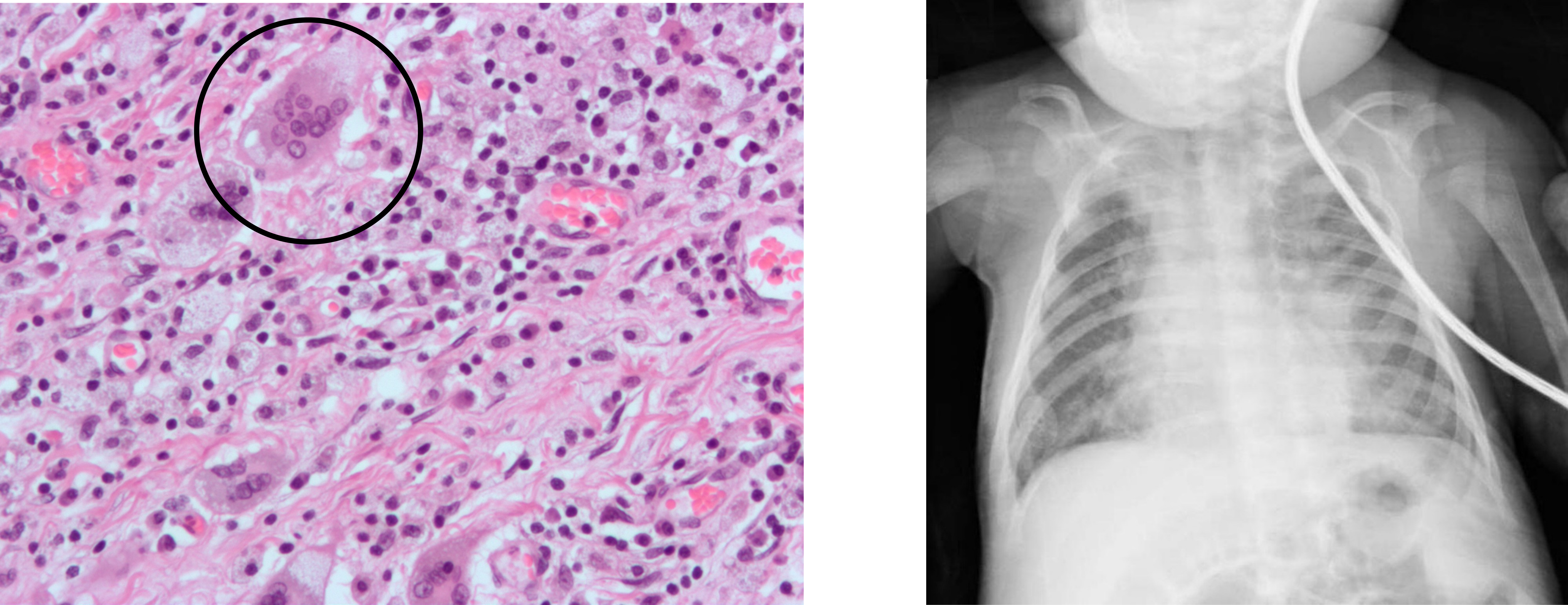
Infection starts in the nasopharynx and then progresses to the epithelium of the bronchioles that appears particularly susceptible to RSV infection. Immune cells are called to the area, but the predominant feature of the infection is the sloughing of the bronchiolar epithelium and the appearance of syncytial giant cells in the airway lumen, as seen in the insert of the histology slide in figure 3.2. With anatomically smaller bronchioles, infants are susceptible to this epithelial sludge blocking the airway. The hallmark of the infection reflects the obstructive nature of the disease with hyperinflation.
The young patient will likely present with a recent history of cough and hallmarks of shortness of breath such as use of accessory muscles. A scattered wheeze is likely, and in severe cases the child develops an expiratory grunt.
Unresolved the RSV can spread to type 1 and 2 pneumocytes through cell-to-cell transmission. There is a high incidence of apnea associated with RSV infection, presumably due to the virus activating defensive reflexes associated with the larynx.
Pneumonia
Now we will look at the consequences of infection of the terminal airways and what is referred to as pneumonia. Although pneumonia can result from infection by one of any number of pathogens, we will first look at a generalized pathophysiological mechanism.
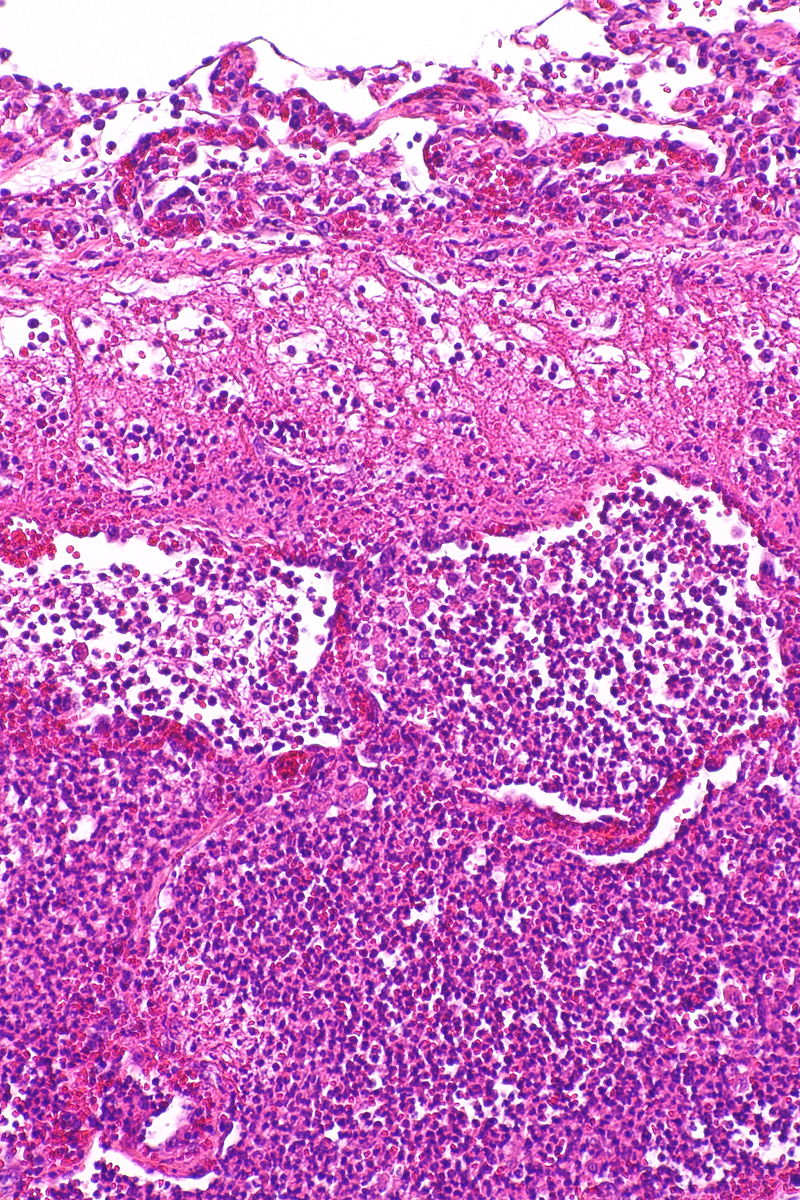
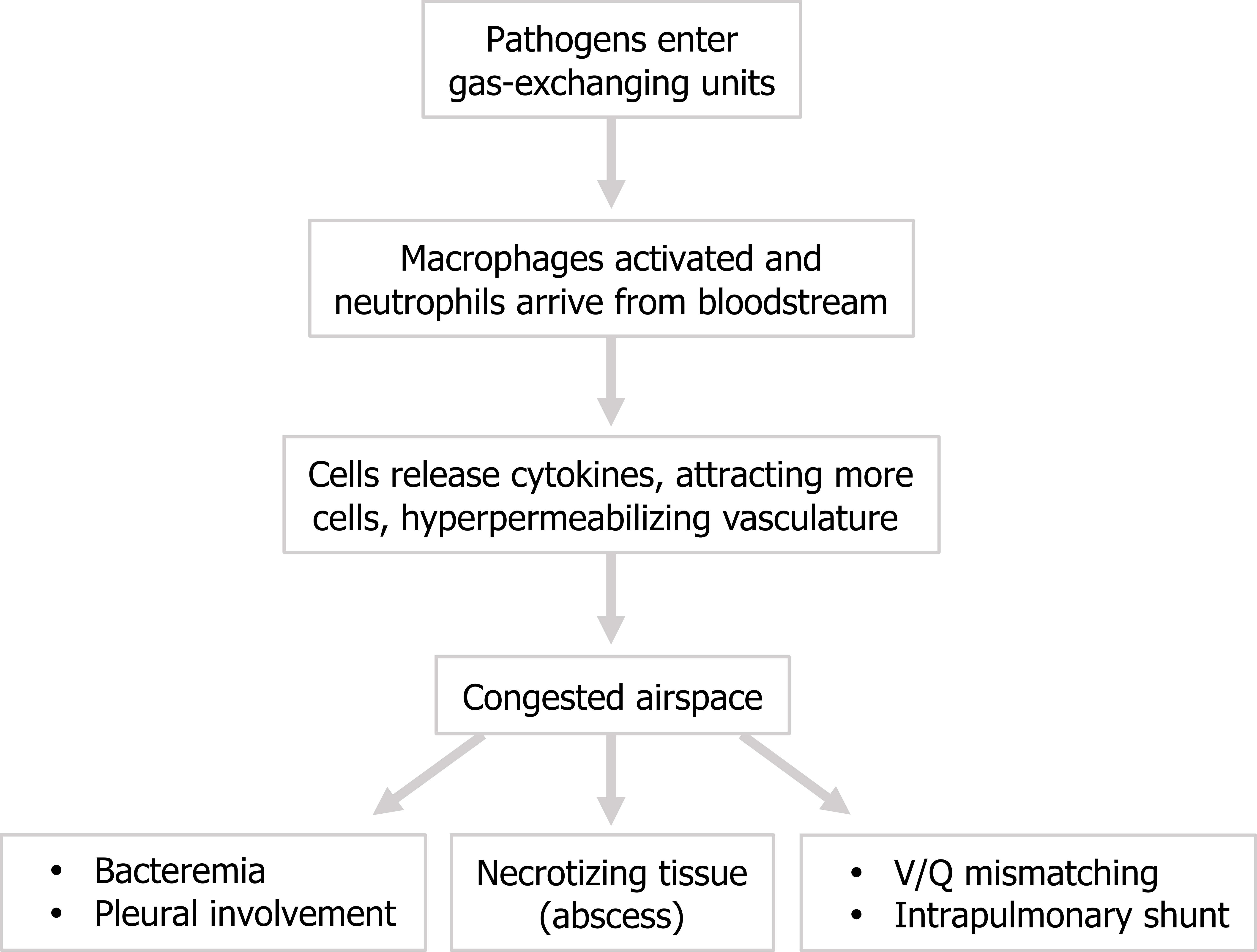
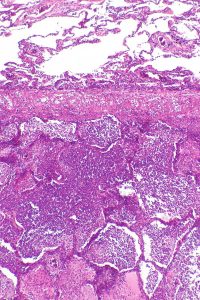
The pathogen arrives in the alveolar space causing activation of alveolar macrophages and recruitment of neutrophils from the bloodstream. These first responder cells release cytokines to attract more neutrophils and hyperpermeabilize the vasculature. Consequently the airspace becomes congested with pathogens, neutrophils, and exudate and incapable of being ventilated (figure 3.3). This produces V/Q mismatching in the effected area and the potential for the establishing of intrapulmonary shunts.
The infection may not be retained by the airway structure and can penetrate the pleural space, in which case an effusion is likely.
The pneumonia-causing pathogen can often be found in blood analysis but the patient remains asymptomatic, but if the infection becomes more established significant signs and symptoms of bacteremia arise.
An infection may lead to necrotized tissue and formation of an abscess in the lung. The prevalence of this is mostly dependent on the pathogen; for example, a tuberculosis infection is famous for causing walled-off abscesses (or granuloma) that try to contain the mycobacterium. These processes are summarized in figure 3.4.
Classification of Pneumonia
The causes of pneumonia are many, but so are the ways in which they are classified. Pneumonias are distinguished by:
- where the patient became infected,
- where in the lung the infection is established, and
- where the pathogen resides at a cellular level.
Typical or atypical pneumonia: We can start at arguably the least clinically helpful classification, the microscopic location. Pneumonias can be either typical or atypical. Typical pneumonium involves the presence of pathogens and immune cells in the airspace, whereas atypical has the pathogen and inflammatory response within the alveolar walls and interstitium (table 3.1). The site is usually dictated by the mode of the pathogen, with typical pneumonia being bacterial and atypical being caused by virus or mycobacterium that are capable of entering cells.
The two forms can have different signs and symptoms with typical pneumonia having a more rapid onset and atypical being more gradual. Both can be associated with fever, but extrapulmonary features such as headache, joint and muscle pain, and nausea are more characteristic of atypical pneumonia. Because of the location of the pathogen; typical pneumonia is associated with a productive cough, whereas the cough of atypical pneumonia is dry, as summarized in table 3.1.
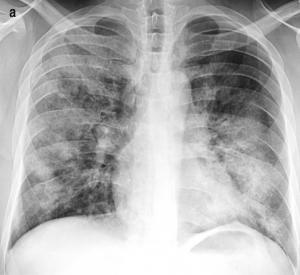
On x-ray the atypical pneumonia shows more diffuse patchy markings associated with the infiltrated interstitium, whereas an x-ray of typical pneumonia shows lobar opacities caused by consolidated airspaces (table 3.1).
| Typical pneumonia | Atypical pneumonia |
|---|---|
 |
 |
| - Airspace involvement - Bacterial - Rapid onset - Few extrapulmonary features - Productive cough |
- Interstitial involvement - Viral/mycoplasma - Gradual onset - Extra-pulmonary features - Dry cough |
 |
 |
Table 3.1: Comparison of typical and atypical pneumonia.
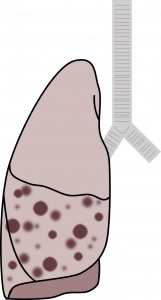
Bronchopneumonia or lobar pneumonia: The next classification is based on the infection’s gross location—whether it occurs in a bronchiolocentric pattern to produce bronchopneumonia, or whether the consolidation occurs in continuous airspaces to occupy a lobe to produce lobar pneumonia. Bronchopneumonia will produce distinct areas of infiltrate, and the chest x-ray will reflect this with opacities following the effected airways (table 3.2). Lobar pneumonia will involve dense consolidation outlining the whole lobe and the possibility of air brochograms as air-filled bronchi are surrounded by the infiltrated, more dense alveoli (table 3.2). Bronchopneumonia is usually bilateral, whereas lobar pneumonia tends to be unilateral. However, both can exist in the same patient, as is the case in the example x-ray in table 3.2.
| Bronchopneumonia | Lobar pneumonia |
|---|---|
 |
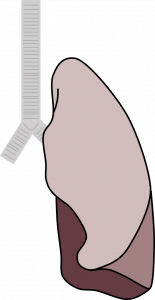 |
| - Multiple distinct foci around bronchioles - Usually bilateral |
- Dense consolidation (air bronchograms) - Usually unilateral |
 |
 |
Table 3.2: Comparison of bronchopneumonia and lobar pneumonia.
Hospital-acquired or community-acquired pneumonia: The last classification relates to the setting in which the infection was acquired, either out in the community or during hospitalization. This classification can provide clues to identifying the pathogen involved. By far the most common cause of community-acquired pneumonia is Streptococcus pneumoniae. Other pathogens can be responsible but tend to affect only those with an underlying condition or characteristic; they are listed in table 3.3 with the usual instigating issue in parentheses. Legionella-related pneumonia requires exposure to laced water droplets, and mycoplasma infection tends to affect young adults living in close quarters, such as military barracks or college dorms. Lastly, and more uncommonly, the pneumonia may be caused by a viral infection.
Hospital-acquired pneumonia is defined as occurring at least three days after hospitalization. Unlike community-acquired pneumonias the pathogen is frequently a gram-negative bacteria or staphylococci that normally would not be able to become established in the lung. However, the hospitalized patient’s weakened state of health, state of consciousness, exposure to poor sterile technique for intubation, or antibiotic therapy can provide these listed pathogens an opportunity (table 3.3).
| Community-acquired | Hospital-acquired - Contracted >3 days of hospitalization - Gram-negative bacteria and staphylococci - Patient is in poor health - Poor state of consciousness (aspiration) - Defective defense mechanisms - Poor antibiotic therapy |
|---|---|
| Streptococcus pneumoniae | Escherichia coli |
| Haemophilus influenzae (COPD) | Enterobacter |
| Moraxella catarrhalis (COPD) | Proteus |
| Klebsiella pneumoniae (alcoholics) | Serratia |
| Staphylococcus (infants, IV drug abuse) | Haemophilus influenzae |
| Escherichia coli (alcoholics, diabetics) | Pseudomonas |
| Legionella pneumophila (water droplets) | Acinetobacter |
| Mycoplasma pneumoniae (young adults) | Staphylococcus |
| Influenza, varicella zoster, adenovirus | Streptococcus pneumoniae |
| Klebsiella pneumoniae |
Table 3.3: Comparison of community- and hospital-acquired pneumonias.
Clinical Findings of Pneumonia
The clinical findings depend on the severity of the infection and underlying cause. Onset can be abrupt or gradual, and is often preceded by upper airway symptoms and associated with malaise, fever, or chills. As the infection progresses cough is established and chest pain and dyspnea can develop.
As the infection progresses expectoration increases and can be purulent or even blood tinged. Mental confusion can arise particularly in elderly or alcoholic patients. If there is multiple lobe involvement then dyspnea can become severe and cyanosis may arise as intrapulmonary shunts become established and more significant. The hypoxemia can be accompanied by hypocapnia as the patient hyperventilates due to the hypoxic drive to breathe.
Chest exams can have variable findings but may include poor respiratory excursion. The consolidated lung fields result in dullness to percussion and a reduction in breath sounds and increase in tactile fremitus. Inspiratory crackles may be heard. With continued progression arterial hypoxia worsens and arterial CO2 falls due to hyperventilation.
Chest x-ray allows the areas of consolidation to be seen, but typically there is no volume loss, which allows pneumonia to be distinguished from atelectasis (although pneumonia and atelectasis can co-occur). Particularly in the case of a typical pneumonia the complete blood count (CBC) panel will show an elevated white blood cell count. See table 3.4 for summary.
| Onset | Progression |
|---|---|
| Abrupt or gradual | Expectoration—purulent, blood tinged |
| Upper respiratory symptoms | Mental confusion (elderly or alcoholic patient) |
| Malaise, chills, fever | Dyspnea and cyanosis with multiple lobe involvement |
| Cough | Chest exam (variable): - Poor respiratory excursion - Dullness to percussion - Reduced breath sounds - Tactile fremitus (consolidation) - Inspiratory crackles |
| Chest pain | Opacity on chest x-ray |
| Dyspnea | No volume loss (distinction from atelectasis) |
| Elevated white cell count |
Table 3.4: Summary of the clinical findings of pneumonia.
References, Resources, and Further Reading
Text
Farzan, Sattar, with Doris L. Hunsinger and Mary L. Phillips. “Chapter 3.” In A Concise Handbook of Respiratory Diseases. Reston, VA: Reston Publishing Company, 1978.
Husain, Aliya N. “Chapter 15: The Lung.” In Robbins and Cotran Pathologic Basis of Disease, 9th ed., edited by Vinay Kumar, Abul K. Abbas, and John C. Aster. Philadelphia: Saunders, an imprint of Elsevier Inc., 2015.
Figures
Figure 3.1: Pathophysiology of acute bronchitis. Grey, Kindred. 2022. CC BY 4.0. https://archive.org/details/3.1_20220203
Figure 3.2: Histological and Radiographic findings for an RSV infection. Grey, Kindred. 2022. CC BY-NC-SA 3.0. Added Giant cells1 by Nephron from WikimediaCommons (CC BY-SA 3.0) and Respiratory syncytial virus by Radswiki, T., et al. from https://doi.org/10.53347/rID-11873 (CC BY-NC-SA 3.0). https://archive.org/details/3.2-new
Figure 3.3: Neutrophils, bacteria, and exudate occupy airspaces in a typical pneumonia. Nephron. 2016. CC BY-SA 3.0. “Acute Pneumonia — Intermed Mag” from WikimediaCommons.
Figure 3.4: General pathophysiology of pneumonia. Grey, Kindred. 2022. CC BY 4.0. https://archive.org/details/3.4_20220203
Table 3.1: Comparison of typical and atypical pneumonia. Includes Case 1 by Bell, D., Hacking, C., et al. from https://doi.org/10.53347/rID-68496 (CC BY-NC-SA 3.0), Acute pneumonia – i — low mag by Nephron from WikimediaCommons (CC BY-SA 3.0), Case 2 by Paks, M., Knipe, H., et al. from https://doi.org/10.53347/rID-27535 (CC BY-NC-SA 3.0), and image 1 by Dr Patsy Lill from University of South Carolina School of Medicine’s Microbiologybook.org (Fair use).
Table 3.2: Comparison of bronchopneumonia and lobar pneumonia. Includes Bronchopneumonia by Kindred Grey from Internet archive (CC BY 4.0), Lobar pneumonia by Kindred Grey from Internet archive (CC BY 4.0), X-ray of bronchopneumonia by Franquet T., Chung J.H. from WikimediaCommons (CC BY 4.0), Case 3 by Paks, M., Knipe, H., et al. from https://doi.org/10.53347/rID-26886 (CC BY-NC-SA 3.0).

